Introduction
Cancer treatment has evolved tremendously over the past few decades, moving from traditional chemotherapy and radiation therapies to more targeted and sophisticated approaches.
One of the most promising developments in recent years is the use of bioengineered immune cells, a form of immunotherapy that is transforming the way oncologists fight cancer. This cutting-edge treatment harnesses the body’s own immune system, modifying its cells to better recognize and eliminate cancer cells.
In this blog, we will delve into how bioengineered immune cells are reshaping oncology, offering hope to millions of patients globally.
Immunotherapy, especially with bioengineered immune cells, represents a paradigm shift in cancer treatment. By combining advancements in molecular biology, bioengineering, and medicine, researchers have made great strides in personalizing cancer treatment, improving outcomes for patients who previously had limited options.
As we explore this exciting field, we’ll examine the mechanisms behind bioengineered immune cells, key treatment types, clinical applications, and the challenges still faced in oncology.
1. The Science Behind Bioengineered Immune Cells
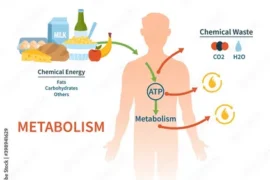
At the core of transforming cancer treatment is the ability to bioengineer immune cells. These cells, primarily T-cells, are genetically modified to enhance their ability to detect and destroy cancer cells.
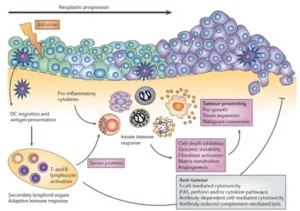
The immune system, in its natural form, is designed to identify and eliminate foreign invaders like bacteria and viruses. However, cancer cells often find ways to evade immune detection by either mimicking normal cells or by creating an immunosuppressive environment.
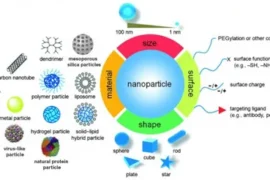
By bioengineering these immune cells, scientists can modify them to better recognize specific markers on cancer cells. One of the most well-known forms of this treatment is chimeric antigen receptor (CAR) T-cell therapy, where T-cells are extracted from a patient’s blood, engineered to express a receptor that binds to specific cancer antigens, and then reintroduced into the body to fight cancer.
This ability to modify immune cells for more effective cancer detection and eradication has made bioengineered treatments a cornerstone of modern oncology. Unlike traditional chemotherapy, which targets both healthy and cancerous cells, these bioengineered cells are precise, minimizing damage to healthy tissue and reducing side effects.
2. Key Forms of Bioengineered Immune Cell Therapies
Cancer treatment using bioengineered immune cells comes in various forms, each with its own advantages and applications. Below are the primary types:
- CAR T-Cell Therapy: As previously mentioned, CAR T-cell therapy is one of the most significant breakthroughs in oncology. Approved for the treatment of certain blood cancers like leukemia and lymphoma, CAR T-cell therapy has demonstrated remarkable success. Patients who once had no viable treatment options have achieved remission, showcasing the transformative potential of this approach. CAR T-cell therapy is now being researched for use in solid tumors, although it has proven more challenging due to the complex environment surrounding these tumors.
- Tumor-Infiltrating Lymphocytes (TILs): TIL therapy involves isolating immune cells that have already entered the tumor but may not be functioning optimally. These cells are extracted, expanded in a lab, and then reinfused into the patient after being activated to attack the tumor more effectively. TILs are particularly promising for melanoma and other cancers with a high mutation burden, as these tumors express a larger number of antigens that immune cells can recognize.
- Natural Killer (NK) Cells: NK cells are a part of the immune system that can destroy cancer cells without prior sensitization. Researchers are exploring ways to bioengineer NK cells to make them more effective in detecting and killing cancer cells. NK cell therapies offer a potential alternative for patients whose T-cells may not be suitable for modification.
These therapies are revolutionizing oncology, offering patients new hope where traditional treatments have failed. The potential for bioengineered immune cells to transform cancer treatment is immense, and ongoing research aims to expand these therapies’ applicability to a wider range of cancers.
3. Clinical Successes and Ongoing Research
One of the most compelling aspects of bioengineered immune cell therapy is the tangible success seen in clinical trials. CAR T-cell therapy, in particular, has produced remission in patients with advanced blood cancers who had no other treatment options. For instance, the FDA approved the first CAR T-cell therapy in 2017 for the treatment of pediatric acute lymphoblastic leukemia (ALL), a significant milestone in cancer treatment.
Additionally, research continues to explore the potential of bioengineered immune cells in treating solid tumors, which present a different set of challenges compared to blood cancers. Solid tumors have an immunosuppressive microenvironment, making it harder for immune cells to penetrate and attack them. However, advancements in combination therapies—such as using checkpoint inhibitors alongside bioengineered immune cells—are showing promise.
The global research community is dedicated to expanding the effectiveness and accessibility of bioengineered immune cell therapies. Clinical trials are underway for different types of cancer, including lung, breast, and ovarian cancers, as well as exploring ways to reduce costs and improve safety.
4. Challenges in Transforming Oncology with Bioengineered Cells
Despite the remarkable potential of bioengineered immune cells in cancer treatment, several challenges remain. These include:
- Cost: Bioengineered therapies like CAR T-cell treatments are extremely expensive, often costing hundreds of thousands of dollars per patient. While these therapies can be life-saving, their high cost limits accessibility, especially in low-income regions. Ongoing efforts to reduce the cost of manufacturing and delivering these treatments are critical for making them more widely available.
- Toxicity and Side Effects: While bioengineered immune cell therapies are generally more targeted than chemotherapy, they are not without risks. Some patients experience cytokine release syndrome (CRS), a potentially life-threatening condition caused by an overactive immune response. Managing these side effects is an essential aspect of improving the safety of these therapies.
- Resistance and Relapse: Although bioengineered immune cells can produce lasting remissions, some patients develop resistance to the treatment or relapse over time. Cancer cells can evolve to evade even the most sophisticated immune responses, underscoring the need for continual advancements in treatment strategies.
Despite these challenges, the progress made in transforming oncology with bioengineered immune cells is undeniable. With every new breakthrough, the future of cancer treatment becomes brighter, offering more personalized, effective, and less invasive solutions.
Conclusion
The integration of bioengineered immune cells into cancer treatment represents one of the most exciting developments in oncology today. From CAR T-cell therapy to natural killer cell therapies, these innovations are reshaping how we approach cancer, offering new hope to patients who had previously run out of options.
While challenges such as cost and resistance remain, the ongoing advancements in research hold the promise of a future where cancer is not only treatable but curable for many more patients.
As bioengineered immune cells continue to transform the landscape of cancer treatment, we are witnessing a shift toward personalized medicine that targets cancer at its root, minimizing harm to healthy tissue and improving patient outcomes. The future of oncology is bright, with bioengineering at the forefront of this transformation.
What do you think about the role of bioengineered immune cells in transforming cancer treatment? We’d love to hear your thoughts, so feel free to leave a comment below!