Heart disease is one of the leading causes of death globally, responsible for millions of lives lost each year. As medical science advances, new avenues for treatment and prevention continue to emerge.
One of the areas receiving increasing attention is the role of platelet activation proteins in combatting heart disease mortality. Understanding the function of these proteins in relation to blood clotting, inflammation, and cardiovascular health opens up new possibilities for reducing mortality from heart disease.
In this blog post, we’ll delve into how platelet activation proteins contribute to heart disease, examine the mechanisms behind their effects, and explore the potential for future therapies. We’ll also look at current research and discuss how targeting these proteins may revolutionize heart disease treatment.
What are Platelet Activation Proteins?
Platelets, the smallest type of blood cells, play an essential role in blood clotting and wound healing. They respond to blood vessel injury by sticking to the affected area and forming clots to prevent blood loss.
However, platelets do much more than clot formation. When they encounter a vascular injury, they release various proteins and signaling molecules that regulate inflammation, immune response, and tissue repair. These proteins are known as platelet activation proteins.
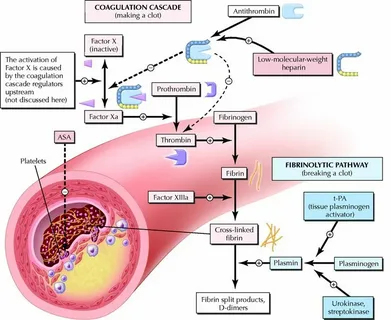
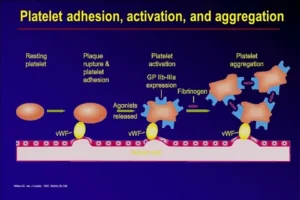
The primary function of platelet activation proteins is to mediate the process that leads to clot formation (thrombosis). They signal to the platelets to aggregate and form clots. In healthy individuals, this process helps to prevent excessive blood loss. However, in individuals with cardiovascular conditions, the same mechanism can lead to harmful outcomes, such as heart attacks and strokes.
Understanding how platelet activation proteins work is vital for combatting heart disease mortality. Their role is crucial not only in initiating clot formation but also in modulating vascular function and the immune response. As a result, they have become a target for therapies designed to reduce heart disease-related deaths.
The Link Between Platelet Activation and Heart Disease
Platelets play a double-edged role in cardiovascular health. While their primary function is protective, they can also contribute to heart disease when overactivated. In cases of atherosclerosis—a condition where fatty deposits (plaques) accumulate on the artery walls—platelets play a role in exacerbating the condition. When the plaque ruptures, platelets are quickly activated to form a clot, which can block the artery and lead to a heart attack or stroke.
One of the key platelet activation proteins involved in this process is glycoprotein IIb/IIIa. When platelets are activated, glycoprotein IIb/IIIa is expressed on their surface, allowing them to bind to fibrinogen and other clotting factors, which leads to clot formation. In cases of heart disease, the overexpression of this protein can result in excessive clotting, increasing the risk of fatal cardiovascular events.
Additionally, P-selectin is another platelet activation protein that plays a pivotal role in the development of atherosclerosis. It mediates the interaction between platelets and the endothelium (the inner lining of blood vessels), which is a critical factor in the formation of atherosclerotic plaques. By facilitating the adhesion of platelets to the vascular wall, P-selectin contributes to inflammation and the progression of heart disease.
By targeting these platelet activation proteins, researchers hope to find ways to reduce clot formation and inflammation in heart disease patients. This approach holds the potential to significantly decrease heart disease mortality by preventing heart attacks and strokes.
Mechanisms of Platelet Activation in Cardiovascular Disease
To understand how platelet activation proteins contribute to heart disease, it is important to explore the underlying mechanisms. When platelets are activated, a complex series of events occurs, including changes in platelet shape, the release of signaling molecules, and the expression of surface receptors that promote clot formation. This process is tightly regulated under normal conditions, but in the context of cardiovascular disease, it can become dysregulated.
Thromboxane A2 (TXA2) is a key molecule in platelet activation. When platelets are exposed to vascular injury or inflammation, TXA2 is produced, triggering platelet aggregation and vasoconstriction. The increased platelet aggregation can contribute to the formation of clots within the arteries, leading to ischemic events such as heart attacks. Drugs that inhibit the production of thromboxane A2, such as aspirin, have been shown to reduce the risk of heart attacks by preventing excessive platelet activation.
ADP receptors on the surface of platelets are another critical component in the activation process. When ADP binds to these receptors, it triggers a signaling cascade that promotes platelet aggregation. Antiplatelet drugs, such as clopidogrel, work by blocking these receptors, thereby reducing the likelihood of clot formation in individuals at risk for heart disease.
Additionally, serotonin released by activated platelets contributes to vasoconstriction and further platelet aggregation. By understanding how these different signaling molecules and receptors contribute to platelet activation, researchers can develop targeted therapies aimed at reducing heart disease mortality.
Current and Emerging Therapies Targeting Platelet Activation
Given the pivotal role of platelet activation in heart disease, a number of therapies have been developed to mitigate its harmful effects. Antiplatelet drugs, such as aspirin, clopidogrel, and newer agents like ticagrelor and prasugrel, are commonly used to reduce platelet activation and lower the risk of heart attacks and strokes. These drugs work by inhibiting various platelet activation pathways, such as the thromboxane or ADP receptor pathways.
However, while current antiplatelet therapies have proven to be effective, they also come with potential side effects, such as an increased risk of bleeding. This has led to ongoing research into more selective therapies that can target platelet activation proteins without causing widespread suppression of platelet function. For instance, monoclonal antibodies that specifically target glycoprotein IIb/IIIa or P-selectin are being explored as potential treatments for heart disease.
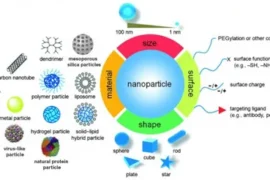
Additionally, researchers are investigating the role of platelet-derived microparticles (PMPs), which are small vesicles released by activated platelets. These microparticles carry pro-inflammatory and pro-thrombotic molecules and are thought to play a role in the development of atherosclerosis. Targeting PMPs could represent a novel therapeutic approach for combatting heart disease mortality.
The future of heart disease treatment may also lie in the use of gene therapies that regulate the expression of platelet activation proteins. By manipulating the genes that control platelet function, it may be possible to reduce the risk of excessive clot formation while preserving the protective role of platelets in wound healing.
Conclusion: The Future of Platelet Activation Research
Platelet activation proteins are at the forefront of research aimed at combatting heart disease mortality. These proteins play a central role in the development of cardiovascular disease by promoting clot formation, inflammation, and plaque formation. By targeting these proteins, researchers hope to develop new therapies that can reduce the incidence of heart attacks and strokes while minimizing the side effects associated with current treatments.
As research continues, the potential for more selective and personalized therapies becomes increasingly promising. Whether through antiplatelet drugs, monoclonal antibodies, or gene therapies, targeting platelet activation proteins holds great potential for saving lives and reducing the global burden of heart disease.
Have you had any experience with antiplatelet therapies, or do you have thoughts on the future of heart disease treatment? Feel free to leave a comment below and share your perspective!